Learn what the labrum is, how labral tears occur, common symptoms, how we evaluate them, treatment options, and expected recovery steps. If you have specific questions, talk with your OrthoNJ provider about your situation and goals.

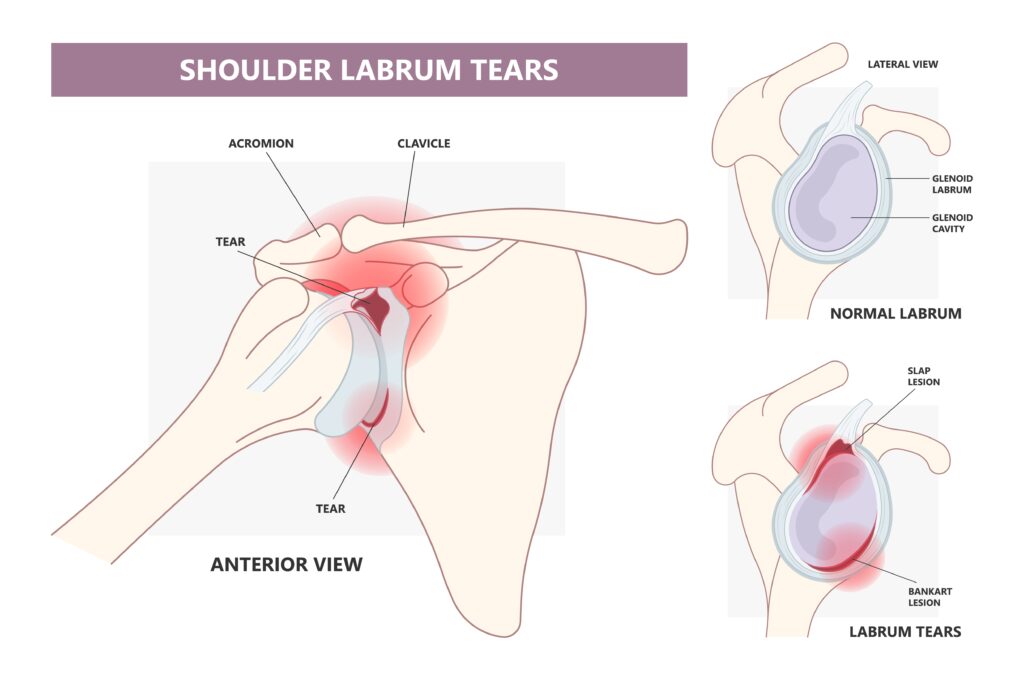
The labrum is a ring of soft cartilage around the edge of the shoulder socket. It deepens the socket and helps the ball at the top of the arm bone stay centered during motion.
Not every change seen on imaging causes symptoms. Small fraying or degenerative changes can be common with age. Tears range from minor fraying to larger injuries that affect stability. Many labral tears do not require surgery and can improve with nonoperative care. Treatment is individualized based on your symptoms, exam findings, tear type, age, and activity goals.
Symptoms vary depending on the location and size of the tear, as well as whether the labral injury affects shoulder stability. In some cases, labral changes may appear on imaging with little or no associated pain.
Common symptoms may include:
It’s important to note that these symptoms are not specific to labral tears and can also be caused by other shoulder conditions, such as rotator cuff disease, arthritis, or biceps tendon disorders. To identify the cause, we consider your medical history, perform a thorough physical examination, and review appropriate imaging studies.
We begin with a focused history and physical exam. Your clinician will assess for instability, painful areas, range of motion limits, and how you use the arm during tasks.
Imaging and diagnostic injections add helpful information but must match your symptoms and exam:
The labrum is soft cartilage that deepens the socket and helps keep the arm bone centered. It contributes to stability while allowing a wide range of motion.
Tears can occur for several reasons:
Treatment is individualized and based on your symptoms, activity level, and goals. Many patients improve with conservative (nonoperative) care. Surgery may be considered when pain, loss of function, or shoulder instability persists despite appropriate nonoperative treatment, or when the physical demands of your sport or occupation make surgical repair the better option. Treatment decisions also depend on the type of tear and the quality of the labral tissue.
Conservative treatment often includes:
Many labral tears—particularly degenerative fraying and small tears without instability—improve with this approach. This is supported by AAOS guidelines (2019) and multiple systematic reviews published between 2021 and 2023.
Corticosteroid injections into the shoulder joint may provide short-term pain relief and help patients progress with physical therapy. However, repeated steroid injections carry risks, including weakening of nearby soft tissues, reduced tendon quality, and a small increased risk of infection if surgery is performed soon after an injection. For these reasons, repeated corticosteroid injections are generally limited, and injections are avoided directly into tendons due to the risk of tendon rupture.
Alternative injections, such as local anesthetic injections for diagnostic purposes or platelet-rich plasma (PRP), may be considered in select cases, though clinical evidence supporting their effectiveness remains variable (clinical reviews, 2020–2023).
Surgical treatment is typically performed arthroscopically and may include labral repair using anchors, selective debridement, and, in certain cases, procedures involving the biceps tendon. Common tear patterns include:
The surgical technique is selected based on the tear pattern, tissue quality, patient age, and activity level.

Rehabilitation is essential whether you have surgery or not. A therapist and surgeon will guide staged progress. Stick with the program provided to lower the chance of persistent symptoms or reinjury.
Below are general, tear-specific timelines to set expectations. Individual recovery varies based on tissue quality, age, fitness, job or sport demands, and how well rehabilitation progresses.
Recovery timelines vary depending on the type of injury, treatment chosen, and individual factors. The ranges below reflect typical expectations, but your progress will be guided by pain levels, strength, range of motion, and ongoing assessment by your surgeon and physical therapist.
Symptom improvement often begins within 4 to 12 weeks of physical therapy. Many patients return to light daily activities within 6 to 12 weeks and gradually resume more demanding tasks by 3 to 6 months, provided progress continues.
(Trimming of frayed labral tissue)
Gentle motion and physical therapy usually begin soon after surgery. Many patients resume light activities within 4 to 8 weeks and return to more strenuous work or sport within 8 to 12 weeks, depending on activity demands and pain control.
(Labral repair near the biceps anchor)
Recovery varies based on activity level:
(Repositioning the biceps tendon)
For many patients—particularly those over approximately 40 years of age, or when the biceps tendon is degenerated or labral tissue quality is poor—biceps tenodesis may be recommended instead of SLAP repair. In some studies, this approach offers reliable pain relief and a faster return to function. Typical recovery includes:
Individual recovery plans may vary.
(Instability following shoulder dislocation)
Sling protection is commonly used, followed by gradual restoration of motion and strengthening. Many patients return to light activities within 8 to 12 weeks and resume contact sports or high-demand activities by 4 to 6 months, based on stability testing and sport-specific demands.
Recovery timelines are similar to other labral repairs. Many patients return to most activities by 4 to 6 months, with a slower progression for sports or activities that place higher stress on the repaired area.
These timelines are general guidelines. Returning to activity too early may increase the risk of repair failure. Your care team will provide individualized milestones based on your recovery and specific goals.
Injections can be diagnostic or therapeutic. A diagnostic local anesthetic injection into the joint can confirm whether the joint is the main pain source. Corticosteroid injections may reduce inflammation and help you participate in therapy.
Important safety points
Choosing SLAP repair versus biceps tenodesis is a common decision point. The choice depends on patient age, activity level, tear pattern, and biceps tendon quality.
Call your doctor if you have any of the following:
If you are unsure what to do, OrthoNJ can evaluate your shoulder and recommend next steps that match your goals.
We cannot promise a specific cure or exact timeline. Imaging must be interpreted together with your symptoms and physical exam. Some labral changes are age-related and may not cause pain. Many tears do not require surgery. Treatment is individualized and guided by your goals, exam findings, and response to therapy.
This page is for education and is not a substitute for personalized medical advice. Talk with your OrthoNJ provider about what is right for you.
If shoulder pain limits work or sport, schedule an exam with OrthoNJ. We will review your history, examine the shoulder, and suggest imaging or a treatment plan tailored to your needs.
Conservative care helps many people, and timely evaluation can prevent further problems and help you return to activities you enjoy. Schedule an exam to start a plan with us.
No. Many tears improve with activity modification, structured physical therapy, and selective injections. Surgery is considered when appropriate nonoperative care does not control pain or when instability or activity demands make repair the better option.
Arthroscopic labral repair is generally safe. Risks include infection, stiffness, reaction to anesthesia, persistent symptoms, and the possibility that the repair does not relieve symptoms. Your surgeon will discuss risks specific to you.
Return to throwing varies widely. Many athletes use a staged throwing program guided by therapists and trainers. Nonelite athletes may return to throwing at 4 to 6 months after some repairs. High level overhead athletes often need 6 to 9 months or longer depending on the repair type and progress.
Ready to talk about your shoulder? Schedule an exam with OrthoNJ, and we will help you understand the best next steps for your goals.
Contact one of OrthoNJ's locations spread out through all of New Jersey.

This treatment info is for informational purposes only. Treatment and recovery vary person to person, and you should consult with your treating physician and team for details on your treatment and recovery process.