This article outlines the major muscles of the leg, how they help you move, common injuries, practical strengthening and stretching guidance with evidence based ranges and progression, and red flag symptoms that require urgent evaluation. It is written for patients and families and includes information relevant to OrthoNJ care.
Your legs contain multiple layers of muscles that work together so you can stand, walk, run, jump, and climb. Understanding the main muscle groups, their locations, and their roles helps you understand pain, choose the right exercises, and discuss care with your OrthoNJ team.
Basic anatomic descriptions below follow standard clinical sources (Gray's Anatomy; Clinical Anatomy by Moore) and use common clinical terms for clarity.
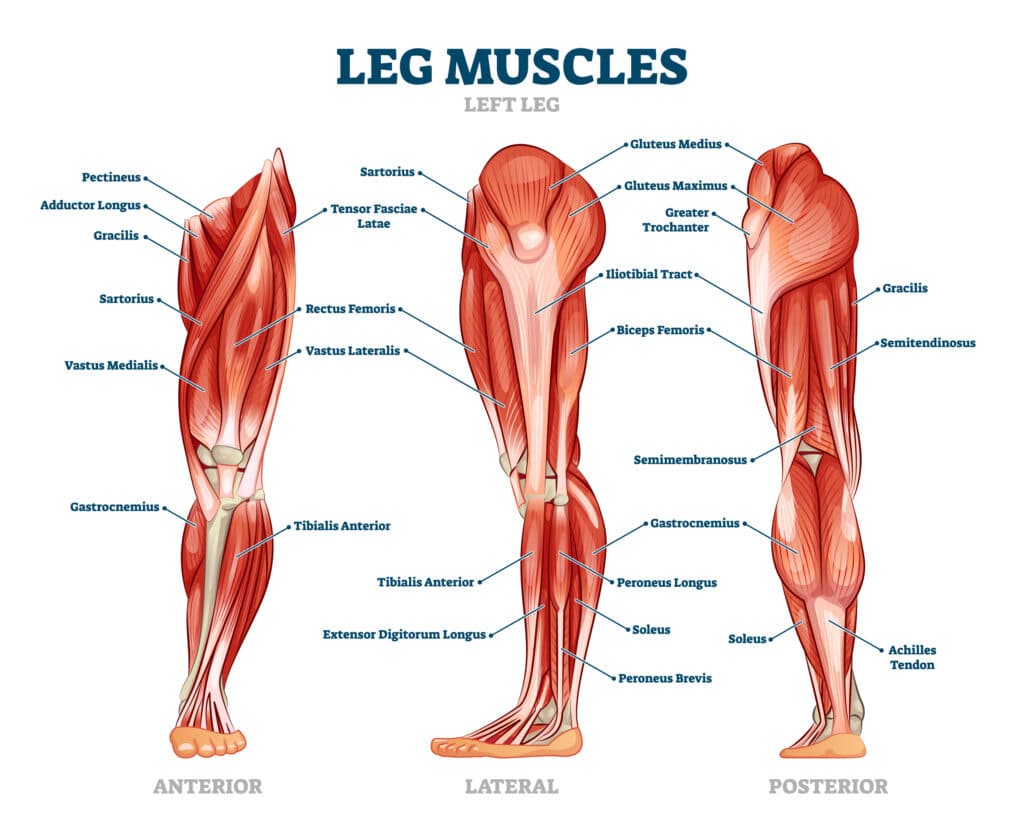

Clinically we divide the lower limb into regions: hip and buttock, anterior thigh, posterior thigh, medial thigh, and the lower leg (anterior, lateral, and posterior compartments). Each group contains muscles with specific actions at the hip, knee, ankle, and foot (Gray's Anatomy; Clinical Anatomy by Moore).
| Muscle group | Representative muscles | Location and main role |
|---|---|---|
| Hip extensors | Gluteus maximus | Buttock. Powerful hip extension for rising from a chair, stair climbing, and sprinting. |
| Hip abductors | Gluteus medius, gluteus minimus, tensor fasciae latae | Lateral hip. Stabilize the pelvis during single leg stance and walking. |
| Hip flexors | Iliopsoas (psoas major, iliacus), rectus femoris, sartorius | Anterior hip and upper thigh. Flex the hip to lift the thigh forward for stepping and climbing. |
| Quadriceps femoris | Rectus femoris, vastus lateralis, vastus medialis, vastus intermedius | Anterior thigh. Extend the knee for standing, walking, and jumping. Rectus femoris also helps hip flexion. |
| Hamstrings | Semimembranosus, semitendinosus, biceps femoris (long and short heads) | Posterior thigh. Knee flexion and assist hip extension; important in deceleration and sprinting. |
| Adductors | Adductor longus, brevis, magnus, gracilis, pectineus | Medial thigh. Draw the leg toward the midline and assist hip stability. |
| Calf and posterior lower leg | Gastrocnemius (medial and lateral heads), soleus, plantaris, tibialis posterior | Posterior lower leg. Plantarflex the ankle to point the foot and provide push off during walking and running; tibialis posterior supports the arch and aids inversion. |
| Anterior lower leg | Tibialis anterior, extensor hallucis longus, extensor digitorum longus | Front of shin. Dorsiflex the ankle to clear the foot during swing and control foot placement at heel strike. |
| Lateral lower leg | Fibularis (peroneus) longus and brevis | Lateral ankle. Evert the foot and provide lateral ankle stability. |
Muscle problems arise from sudden overload, repeated strain, direct impact, or chronic overuse. Specific patterns are common: hamstring strains in sprinting, quadriceps or patellar tendinopathy in jumping athletes, calf strains with push off, and anterior compartment overuse such as shin splints. Tendinopathy and muscle strains are common and may need graded loading and time to recover (Clinical sports medicine texts).
Balanced strength and flexibility reduce injury risk and improve function. Use a progressive approach: start with pain guided, low load exercises and advance load and complexity over weeks as tolerated. General exercise prescription is based on strength training principles and clinical rehabilitation guidelines.
Certain symptoms require prompt medical evaluation. Contact OrthoNJ or seek urgent care if you experience any of the following.
If you have any of these signs, seek prompt evaluation. OrthoNJ can assess for urgent conditions, order imaging or vascular studies if needed, and arrange immediate treatment.
Many muscle strains and overuse injuries improve with activity modification, progressive rehabilitation, and time. Some conditions require additional treatments such as injections, vascular or compartment interventions, or surgery. Your OrthoNJ provider will explain options and an expected recovery timeline based on the specific diagnosis.
Recovery depends on severity. Mild strains often improve in 2 to 6 weeks with guided therapy. Moderate to severe tears can take several months and sometimes need imaging or surgical evaluation. Progress follows pain control, regained range of motion, and progressive strength milestones.
Light activity and gentle stretching are often safe and helpful for mild discomfort, but avoid exercises that increase sharp or worsening pain. Use pain as a guide and consult OrthoNJ for a tailored plan if symptoms persist or limit function.
If leg pain limits daily activities, work, or sport, schedule an exam with OrthoNJ. We will review your history, perform a focused physical exam, and recommend imaging or a rehabilitation plan when appropriate.
Early evaluation helps most people get the right care and return to the activities they enjoy.
Contact one of OrthoNJ's locations spread out through all of New Jersey.

This treatment info is for informational purposes only. Treatment and recovery vary person to person, and you should consult with your treating physician and team for details on your treatment and recovery process.