Discover which muscles make up the core, why they matter for pain and movement, how we check core control, and safe ways to get stronger. If you have specific questions, talk with an OrthoNJ provider about your situation.

Your core is more than just the front abdominal muscles. It includes layers of muscles in the front, back, sides, pelvis, and diaphragm. Together these muscles control your spine and pelvis and help you move efficiently.
Core control supports posture, protects the back during lifting, and transfers force between your upper and lower body. Weakness or poor coordination can contribute to back or pelvic pain, but targeted exercise and guidance often improve function.
The core includes several groups of muscles that work together to stabilize the trunk. Below are the main players and a short, plain language description of what they do.
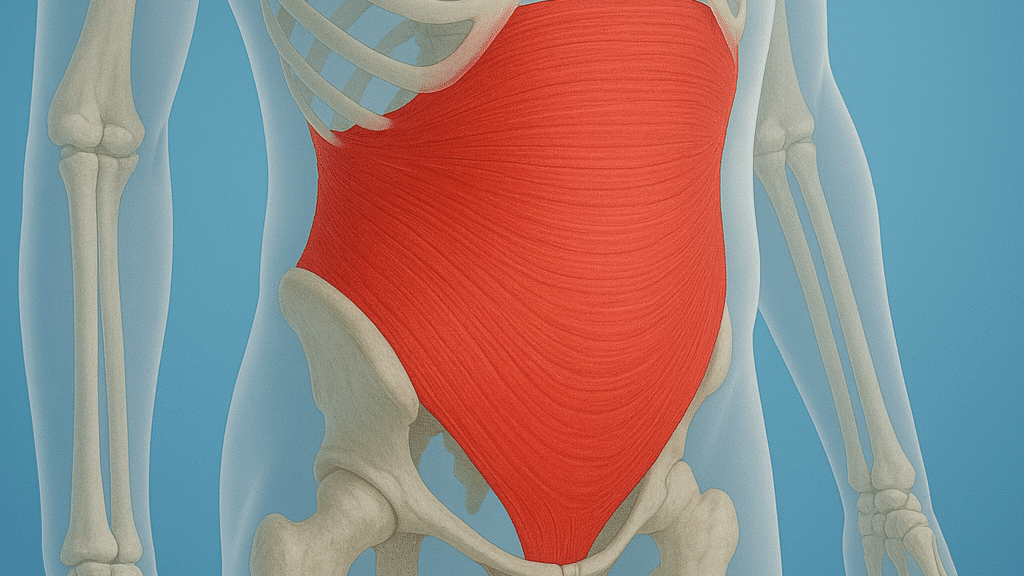
Deep abdominals: The transversus abdominis wraps around the belly and helps steady the spine.
Diaphragm: The main breathing muscle coordinates with the rest of the core to manage pressure inside the chest and abdomen.
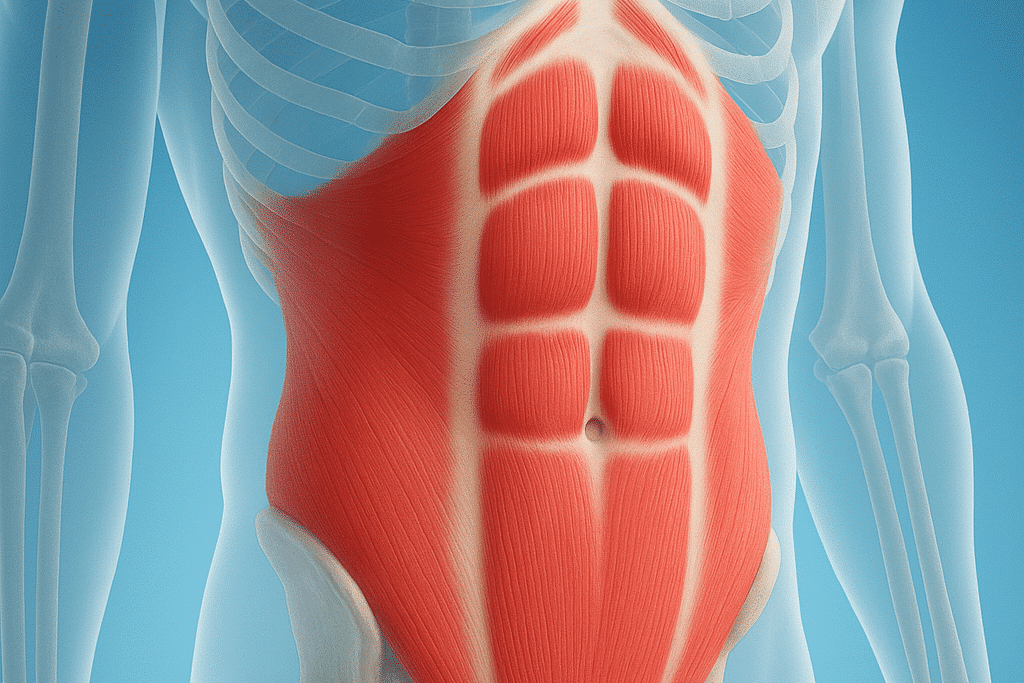
Surface abdominals: The rectus abdominis and obliques help bend and rotate the trunk and support posture.
Pelvic floor: These muscles support pelvic organs and add stability to the base of the trunk.
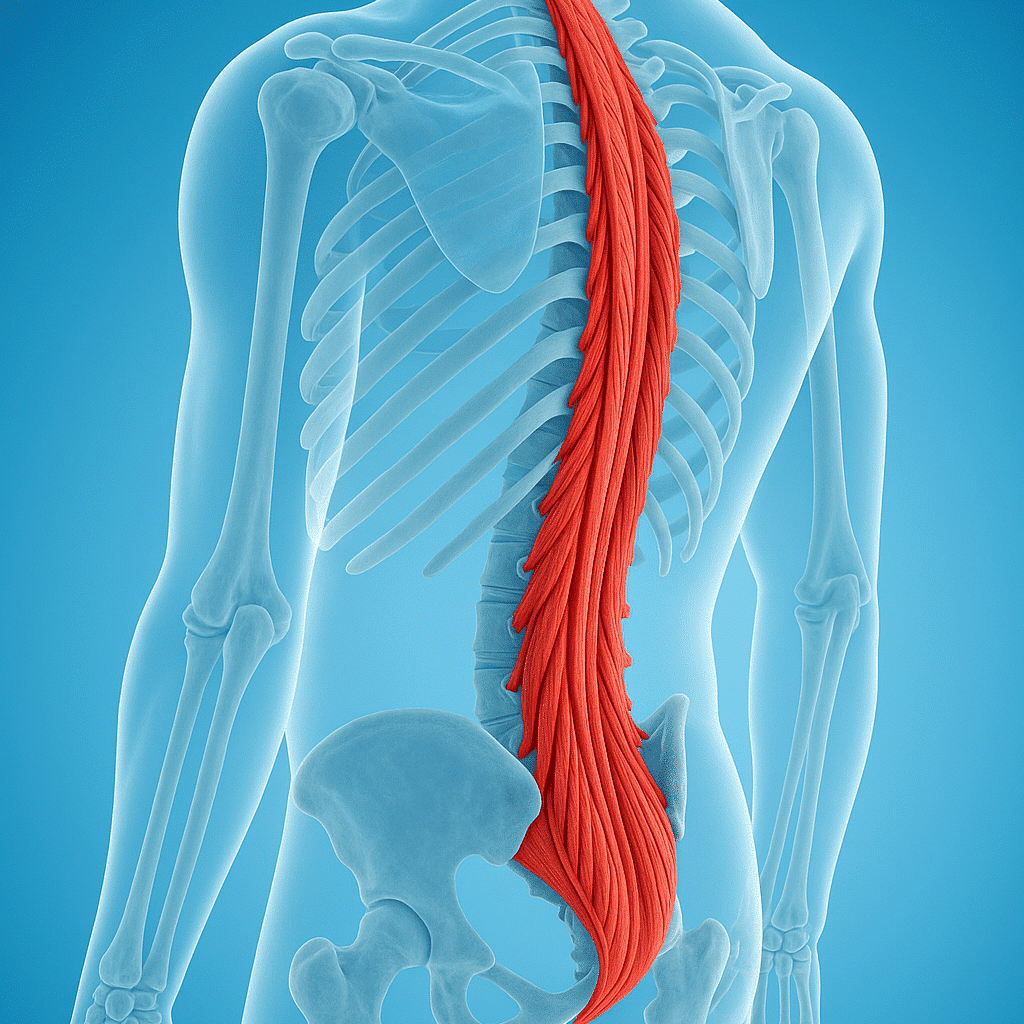
Back muscles: The erector spinae and multifidus support the spine and control small movements between vertebrae.
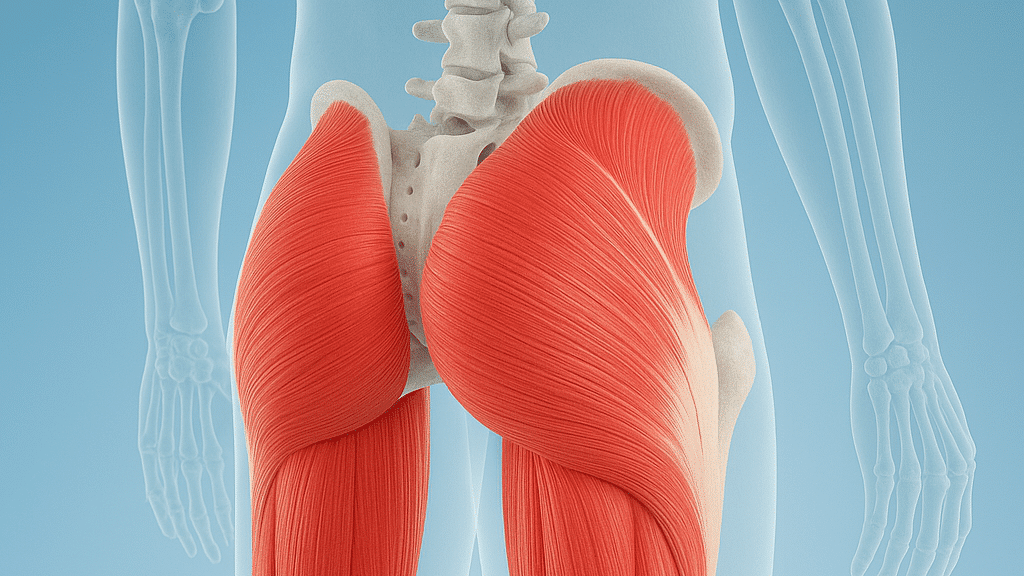
Hip and glute muscles: Strong hips help the core control movement and reduce strain on the lower back.
A well functioning core helps you stand, lift, and move without placing extra stress on the spine. It also improves balance and athletic performance. When core muscles do not activate properly, other muscles or the spine may take too much load, which can cause pain.
Evaluation starts with a focused history and movement exam. We ask how your pain started, what makes it better or worse, and how it affects daily activities. We watch you bend, lift, and stand to look for movement patterns.
Common parts of the exam include tests of:
Imaging such as X ray or MRI may be used when we suspect a structural problem that changes management. Imaging findings often do not correspond to pain, so we interpret tests alongside the exam and your symptoms and make decisions based on the whole clinical picture.
We focus on control first, then endurance, and finally functional movement. That means learning to activate deep muscles without holding your breath, building endurance with repeated, controlled holds, then practicing the movements you need for work or sport.
Transversus abdominis activation should be performed with normal breathing and without breath holding. A useful cue is a gentle drawing in of the lower belly toward the spine while breathing normally and avoiding tensing the neck, shoulders, or glutes. Avoid Valsalva or forceful breath holds, especially if you have high blood pressure, osteoporosis, or are pregnant.
If pain is present, we start with gentle, pain guided progress and work closely with a physical therapist. Exercises are tailored to your needs and advanced only when form and control are reliable.
Clinical guideline based progression commonly follows three stages. Use these as benchmarks to discuss with your therapist.
These stages are guideline based but must be individualized. If performance breaks down or pain increases, return to the prior stage and reassess.
Below are commonly recommended exercises. Start them only after checking with your provider or therapist if you have recent injury, significant pain, pregnancy, or osteoporosis.

Work with a therapist to ensure exercises match your goals. If you are returning from injury we focus on movement quality, then add load and work or sport specific practice. Strengthening the hips and practicing proper breathing often improves results.
Consistency matters. Short, regular sessions most days of the week are better than occasional long workouts. Track progress by pain, function, and the ability to do everyday tasks.
Timelines vary by the cause of your problem and your starting point. Many people see meaningful improvement in a few weeks with guided therapy, while others need longer to reach higher level goals. Care is individualized based on exam findings and goals.
Osteoporosis: Avoid heavy spinal flexion, repetitive impact, and forceful breath holds. Use safer modifications such as shorter lever arms, supported positions, emphasis on hip hinge technique, and progressive loading under therapist supervision.
Pregnancy: Focus on pelvic floor and transversus abdominis activation with normal breathing. Avoid prolonged supine positions after 20 weeks, avoid intense abdominal compression, and consult your prenatal provider or a therapist experienced in prenatal care for exercise modifications.
Call a doctor if you have any of the following:
If you are unsure, schedule an exam with OrthoNJ so we can evaluate your symptoms and outline a safe plan that matches your goals.
No single exercise works for everyone. Progress is gradual and guided by pain, function, and examination findings. Imaging alone does not tell the full story, so we combine tests with the clinical exam to make decisions. Care is individualized to your needs and goals.
This content is for education only and is not a substitute for personalized medical advice. Talk with your OrthoNJ provider about what is right for you.
If core weakness or back pain limits your daily life or activities, schedule an exam with OrthoNJ. We will review your history, perform a focused exam, and recommend imaging or a therapy plan if needed.
Early, targeted care often helps prevent ongoing problems and gets you back to the activities you enjoy.
Strengthening often helps, especially when poor muscle control is contributing to pain. However, some back pain comes from other causes, so we evaluate your individual case and tailor treatment.
A physical therapist can ensure you activate the right muscles, progress safely, and return to activities. Many people benefit from at least a few sessions to learn proper technique.
Contact one of OrthoNJ's locations spread out through all of New Jersey.

This treatment info is for informational purposes only. Treatment and recovery vary person to person, and you should consult with your treating physician and team for details on your treatment and recovery process.