Tendonitis—also spelled tendinitis—refers to the inflammation or irritation of a tendon. This thick fibrous cord connects muscle to bone. While it may sound similar to arthritis, it’s a very different condition. Arthritis affects the joints, while tendonitis affects the tissue that enables muscles to move those joints.
Tendonitis is one of the most common causes of musculoskeletal pain. Whether you're a recreational athlete, a weekend gardener, or someone whose job involves repetitive motion, understanding how and why this condition develops is the first step toward healing and prevention.
Technically? Nothing. Both terms describe the same condition. "Tendinitis" is a variant spelling more commonly used in medical literature, while "tendonitis" is often preferred in general use. At OrthoNJ, we use both depending on the audience, but most importantly—we treat the condition either way!
More broadly, tendonitis is part of a family of tendon disorders known as tendinopathies, which include:
If tendonitis is left untreated or becomes chronic, it can evolve into tendinosis, which is more serious, harder to treat, and slower to heal. That’s why early diagnosis and intervention are essential.
Regardless of profession or activity level, anyone who pushes their tendons beyond their limit without proper support is susceptible.
At OrthoNJ, we help patients understand not only how to treat tendonitis, but why it happens—and how to prevent it from returning. Our orthopaedic specialists, physical therapists, and sports medicine doctors work as a team to evaluate movement patterns, improve biomechanics, and guide recovery plans tailored to each person’s lifestyle and goals.
If you’re noticing early signs of tendon pain, don’t wait until it becomes a chronic issue. Schedule a consultation with an OrthoNJ specialist today.
You don't have to stay in pain. Contact one of our ONJ divisions to schedule an appointment.

Tendonitis is most frequently caused by repetitive stress—performing the same movement over and over again without proper rest or support. This is common in both athletics and occupational tasks.
Other contributing factors include:
As we age, tendons naturally lose moisture and flexibility, making them less able to absorb stress. This increases the chance of micro-tears and inflammation, even from everyday activities.
Incorrect posture or faulty movement patterns—like slouching, awkward lifting, or uneven gait—place uneven stress on tendons, leading to overuse in certain areas and a higher risk of tendonitis.
Using poor form during exercise or sports places excess strain on tendons. Over time, this repeated stress can inflame the tendon and lead to chronic pain, especially if not corrected.
Skipping warm-ups or cool-downs leaves tendons cold, stiff, and more prone to injury. Without proper recovery, tendons don’t have time to heal from stress, increasing the chance of inflammation.
Calcium buildup or bone spurs near tendons can create friction or pressure, irritating the tendon tissue and triggering inflammation, especially during movement.
In rare cases, tendonitis can result from trauma or systemic inflammatory conditions.
While tendonitis can affect anyone, it is more common in adults over the age of 40, because tendons naturally become less flexible and more prone to injury.
Risk can be especially elevated for:
Athletes subject their tendons to high levels of repetitive motion, impact, and mechanical load, often pushing their bodies beyond normal limits. Sports-specific motions—like swinging a racquet or sprinting—target the same tendons over and over, increasing microtrauma and inflammation. Without adequate rest or cross-training, these stressors accumulate and raise the risk of tendonitis.
Laborers often perform physically demanding tasks involving lifting, reaching, or tool use, frequently under time pressure and without ideal ergonomic support. Repetitive use of the same joints throughout long shifts places constant strain on the connecting tendons. This daily wear and tear, especially without proper recovery, significantly raises their risk.
Musicians engage in precise, repetitive finger and wrist movements for hours at a time, often with minimal rest. Tendons in the hands, wrists, and forearms are especially susceptible due to the fine-motor control required and the lack of muscular bulk to absorb stress. Over time, even subtle overuse can result in chronic tendon inflammation.
Office workers may not seem high-risk, but extended typing, mouse use, and poor workstation ergonomics can strain tendons in the hands, wrists, neck, and shoulders. Static posture and repetitive micro-movements without regular breaks reduce blood flow and increase localized tendon stress.
Poor posture—like slouching, forward head tilt, or unsupported sitting—places chronic, uneven stress on tendons, especially in the neck, shoulders, and back. Similarly, poorly arranged workstations or tools force the body into awkward positions that overwork certain tendons without giving them time to rest. Over time, this imbalanced load increases inflammation and raises the risk of developing tendonitis.
Athletes, manual laborers, musicians, and individuals with repetitive motion in their jobs face a significantly higher risk of developing tendonitis. This isn’t just because they’re more active. It’s about how repetitive stress and mechanical overload affect the tendons over time.
What does tendonitis feel like? The hallmark symptom of tendonitis is localized pain, especially when using the affected joint.
Tendonitis is often mistaken for a muscle strain, but there’s a key difference: muscle pain is felt in the body of the muscle, while tendonitis pain is felt near the joint, where the muscle attaches to bone.
Tendonitis primarily occurs in tendons that are near or cross over joints, because these are the areas where tendons are most active and under the most stress during movement. While tendons exist throughout the body, those not involved in joint motion are rarely stressed enough to become inflamed, so tendonitis almost always shows up near joints.
Tendonitis can affect nearly any joint in the body. Some of the most commonly affected areas include:
If you're feeling persistent discomfort in any of these areas, particularly after physical activity or repetitive movement, it may be time to consult an orthopedic specialist.
At OrthoNJ, we believe in personalized, noninvasive care whenever possible. Most cases of tendonitis respond well to conservative treatment, especially when addressed early.
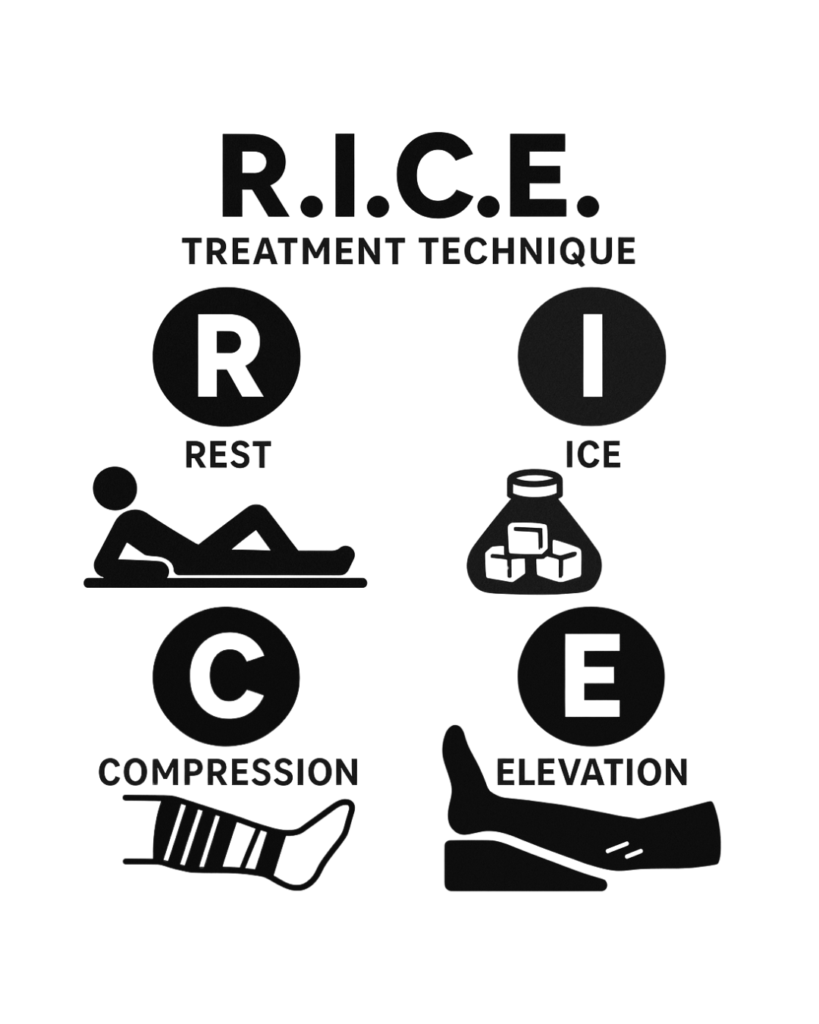
Rest – Avoid aggravating activities
Ice – Apply for 15–20 minutes several times a day
Compression – Use a sleeve, wrap, or brace
Elevation – Keep the area raised above heart level to reduce swelling
Surgical intervention is rare, but may be necessary if:
In these cases, OrthoNJ surgeons leverage fellowship-trained expertise and advanced techniques to remove damaged tissue, restore function, and help patients return to their daily activities.
Prevention is part of our treatment philosophy. To reduce the risk of recurrence, our team recommends:
If your work or sport involves repetitive movement, ask your orthopedic specialist for tips on modifying your form or equipment to reduce stress on your tendons.
As the largest independent orthopedic group in New Jersey, OrthoNJ exists to put patients—not profits—first. Our team of over 100 board-certified, fellowship-trained orthopedic specialists delivers high-touch, personalized care, backed by the collective strength of our regional network.
Whether your tendonitis is new or chronic, complex or straightforward, we bring the Power to Put Patients First—helping you heal faster, move better, and stay active longer.
If you're struggling with joint or tendon pain, don’t wait. Contact an OrthoNJ division near you to schedule an evaluation and take the first step toward relief.